Inflammation, What is it? How to handle it.
 Without inflammation, wounds and infections would never heal. Similarly, progressive destruction of the tissue would compromise the survival of the organism. However, chronic inflammation can also lead to a host of diseases, such as hay fever, periodontitis, atherosclerosis, rheumatoid arthritis, and even cancer (e.g., gallbladder carcinoma). It is for that reason that inflammation is normally closely regulated by the body.
Without inflammation, wounds and infections would never heal. Similarly, progressive destruction of the tissue would compromise the survival of the organism. However, chronic inflammation can also lead to a host of diseases, such as hay fever, periodontitis, atherosclerosis, rheumatoid arthritis, and even cancer (e.g., gallbladder carcinoma). It is for that reason that inflammation is normally closely regulated by the body.
Inflammation can be classified as either acute or chronic. Acute inflammation is the initial response of the body to harmful stimuli and is achieved by the increased movement of plasma and leukocytes (especially granulocytes ) from the blood into the injured tissues. A cascade of biochemical events propagates and matures the inflammatory response, involving the local vascular system, the immune system, and various cells within the injured tissue. Prolonged inflammation, known aschronic inflammation, leads to a progressive shift in the type of cells present at the site of inflammation and is characterized by simultaneous destruction and healing of the tissue from the inflammatory process.
Heart disease, obesity, depression, arthritis (and any -itis, really), autoimmune diseases, insulin resistance – all classics worthy of accolades and all linked to inflammation, sometimes even causally.
Inflammation is part of our innate immunity
Our innate immunity is what is naturally present in our bodies when we are born, and not the adaptive immunity we get after an infection or vaccination. Innate immunity is generally non-specific, while adaptive immunity is specific to one pathogen: What is the difference between chronic inflammation and acute inflammation?
 Acute inflammation – starts rapidly (rapid onset) and quickly becomes severe. Signs and symptoms are only present for a few days, but in some cases may persist for a few weeks.
Acute inflammation – starts rapidly (rapid onset) and quickly becomes severe. Signs and symptoms are only present for a few days, but in some cases may persist for a few weeks.
Examples of diseases, conditions, and situations which can result in acute inflammation include: acute bronchitis, infected ingrown toenail, sore throat from a cold or flu, a scratch/cut on the skin, exercise (especially intense training), acute appendicitis, acute dermatitis, acute tonsillitis, acute infective meningitis, acute sinusitis, or a boil.
 Chronic inflammation – this means long-term inflammation, which can last for several months and even years. It can result from: Failure to eliminate whatever was causing an acute inflammation An autoimmune response to a self antigen – the immune system attacks healthy tissue, mistaking it (them) for harmful pathogens. A chronic irritant of low intensity that persists
Chronic inflammation – this means long-term inflammation, which can last for several months and even years. It can result from: Failure to eliminate whatever was causing an acute inflammation An autoimmune response to a self antigen – the immune system attacks healthy tissue, mistaking it (them) for harmful pathogens. A chronic irritant of low intensity that persists
Examples of diseases and conditions with chronic inflammation include: asthma, chronic peptic ulcer, tuberculosis, rheumatoid arthritis, chronic periodontitis, ulcerative colitis and Crohn’s disease, chronic sinusitis, and chronic active hepatitis (there are many more).
chronic inflammation can eventually cause several diseases and conditions, including some cancers, rheumatoid arthritis, atherosclerosis, periodontitis, and hay fever. Inflammation needs to be well regulated. The five cardinal signs of acute inflammation – “PRISH”
PRISH
Pain – the inflamed area is likely to be painful, especially when touched. Chemicals that stimulate nerve endings are released, making the area much more sensitive.
Redness – this is because the capillaries are filled up with more blood than usual
Immobility – there may be some loss of function
Swelling – caused by an accumulation of fluid
Heat – as with the reason for the redness, more blood in the affected area makes it feel hot to the touch
The five classical signs of inflammation
Dolor – Latin term for “pain”
Calor – Latin term for “heat”
Rubor – which in Latin means “redness”
Tumor – a Latin term for “swelling”
Functio laesa – which in Latin means “injured function”, which can also mean loss of function
Acute and chronic inflammation
The lists below show the difference between chronic and acute inflammation regarding the causative agents, which major cells are involved, features regarding onset, duration, and outcomes:
Acute Inflammation
Causative agents – harmful bacteria or injury to tissue
Major white blood cells involved – mainly neutrophils, basophils (in the inflammatory response), and eosinophils (response to parasites and worms), and mononuclear cells (macrophages, monocytes)
Primary mediators – eicosanoids, vasoactive amines
Onset (when does the inflammation start) – straight away
Duration – short-lived, only a few days
Outcomes – the inflammation either gets better (resolution), develops into an abscess, or becomes a chronic inflammation
Chronic inflammation
Causative agent – non-degradable pathogens that cause persistent inflammation, infection with some types of viruses, persistent foreign bodies, overactive immune system reactions
Major white bloods cells involved – Macrophages, lymphocytes, plasma cells (these three are mononuclear cells), and fibroblasts
Primary mediators – reactive oxygen species, hydrolytic enzymes, IFN-γ and other cytokines, growth factors
Duration – from several months to years
Outcomes – the destruction of tissue, thickening and scarring of connective tissue (fibrosis), death of cells or tissues (necrosis)
Autoimmune disorders and inflammation
 An autoimmune disease, also known as autoimmune disorder, is one where the body initiates an immune response to healthy tissues, mistaking them for harmful pathogens or irritants. The immune response triggers an inflammatory response too.
An autoimmune disease, also known as autoimmune disorder, is one where the body initiates an immune response to healthy tissues, mistaking them for harmful pathogens or irritants. The immune response triggers an inflammatory response too.
There are literally hundreds of autoimmune diseases, and nearly all of them have inflammation as one of the signs, examples include:
Rheumatoid arthritis – there is inflammation in the joins, tissues surrounding the joints, and sometimes some other organs in the body
Ankylosing Spondylitis – there is inflammation of the vertebrae, muscles, ligaments, and also the sacroiliac joints (where the spine and hips meet)
Celiac Disease – there is inflammation and destruction of the inner lining of the small intestine.
Crohn’s Disease – the gastrointestinal tract becomes inflamed. Inflammation is most common in the ileum (small intestine), but may occur anywhere in the GI tract, from the mouth to the anus.
Fibromyalgia – often a set of symptoms related to another autoimmune disorder, such as lupus or rheumatoid arthritis. There is pain in various parts of the body. Location and even the existence of inflammation is unclear.
Graves’ Disease – one of the signs is goiter; when the thyroid gland is inflamed. Exophthalmos, inflammation of the muscles behind the eyes. Grave’s dermopathy, inflammation of the skin, usually the shins and the top of feet (uncommon)
Idiopathic Pulmonary Fibrosis – the role of inflammation is unclear. Experts used to think that the disease was mainly caused by inflammation within the alveoli (tiny sacs within the lungs). However, treatments to reduce inflammation are often disappointing. Therefore, although there is inflammation, its impact on the disease is a bit of a mystery.
Lupus – there can be inflammation in the joints, lungs, heart, kidney and skin.
Psoriasis – there is inflammation of the skin. In some cases, as in psoriatic arthritis, the joints and tissue surrounding the joints may also become inflamed.
Type 1 Diabetes – inflammation in various parts of the body are likely if the diabetes is not well controlled.
Addison’s disease – inflammation of the adrenal glands. The stress to the body caused by this disease can also lead to inflammation elsewhere.
Vaslculitis – refers to a group of disorders in which inflammation eventually destroys blood vessels, both arteries and veins.
Various allergies – all allergies have inflammation. Asthma has inflammation of the airways, in hay fever the nose, ear and throat mucous membranes become inflamed, and people who are allergic to bee stings may have serious life-threatening inflammation which affects the whole body (anaphylaxis).
Vitamin A deficiency – inflammatory responses are much more likely if the person is deficient in vitamin A.
The disorders mentioned above are just a small example of the hundreds of autoimmune disorders which have inflammation as one of their signs.
What are the possible treatments for inflammation?
Some herbs have anti-inflammatory properties
 Harpagophytum procumbens – also known as devil’s claw, wood spider or grapple plant comes from South Africa and is related to sesame plants. European colonists brought devil’s claw back home to treat arthritis, fever and pain. According to the British Herbal Pharmacopoeia, Devil’s Claw has diuretic, sedative and analgesic properties.
Harpagophytum procumbens – also known as devil’s claw, wood spider or grapple plant comes from South Africa and is related to sesame plants. European colonists brought devil’s claw back home to treat arthritis, fever and pain. According to the British Herbal Pharmacopoeia, Devil’s Claw has diuretic, sedative and analgesic properties.
Hyssop Hyssopus – from the plant family Lamiaceae, is added to eau de Cologne and Chartreuse (liqueur drink). It is also used to color some spirits. Hyssop is mixed with other herbs, such as liqourice for the treatment of some lung conditions, including inflammation. Beware of the essential oils of hyssop, as they can lead to life-threatening convulsions in laboratory animals.
Ginger – also known as ginger root, is the mass of roots (rhizome) of the Zingiber officinale plant. It is used as a medicine or a spice. Jamaican ginger was the traditional medical form of this root, and has been used as a carminative (to treat gas or wind) and a stimulant. It has been used for hundreds of years to treat dyspepsia, constipation, colic, other gastrointestinal problems, as well as rheumatoid arthritis pain.
Researchers from Michigan Medical School reported that ginger supplements were found to reduce the markers of colon inflammation. Chronic colon inflammation is associated with a higher risk of developing colon cancer. They added that ginger supplements may help prevent colon cancer.
Turmeric (Curcuma longa) – also a plant of the ginger family. Current research is looking into the possible beneficial effects of turmeric in treating arthritis, Alzheimer’s disease, and some other inflammatory conditions. Curcumin, a substance found in turmeric, is under investigation for the treatment of several illnesses and disorders, including inflammation.
Cannabis – contains a cannabinnoid called cannabichromene, which has been shown to have anti-inflammatory properties.
Other treatments for inflammation
Applying ice – do not place the ice in direct contact with skin, wrap it in a cloth or a purpose-made ice bag. Applying ice has been shown to reduce inflammation. Athletes commonly use ice treatment for managing pain and inflammation. Inflammation can go down more rapidly if you rest, apply ice, compression, and elevate the affected area (have your ankle raised if the swelling is there, for example).
Fish oil (Omega-3) – scientists from Ohio State University Center for Clinical and Translational Science reported on a study in the journal Brain, Behavior and Immunity that the daily consumption of fish oil, omega-3 reduced both inflammation and anxiety in a group of young healthy people.
Green tea – researchers from the Laura W. Bush Institute for Women’s Health at the Texas Tech University Health Sciences Center found that regular green tea drinking enhances bone health and reduces inflammation in postmenopausal women. They added that Tai-Chi appears to have the same beneficial effect.
Tart cherries – sports scientists found that tart cherries have powerful anti-inflammatory properties which may help millions of Americans who suffer from joint pain and arthritis. The team, from Oregon Health & Science University even went as far as saying that “(tart cherries) have the highest anti-inflammatory content of any food”. They believe that tart cherries could help patients with osteoarthritis manage their pain effectively. Twenty females aged from 40 to 70 years drank tart cherry juice twice a day for three weeks; they all suffered from inflammatory osteoarthritis. At the end of the three weeks there were significant falls in levels of key inflammation markers.
Certain foods can promote inflammation in the body by providing the raw materials needed to produce certain inflammatory compounds. These pro-inflammatory foods should only be eaten infrequently and in limited amounts. The University of Wisconsin Department of Integrative Medicine states that high-fat meats and dairy foods contain arachidonic acid, a substance that is needed to form pro-inflammatory compounds in the body. Limit hamburgers, hot dogs, sausage, ribs and other fatty cuts of red meats. Avoid the skin on chicken and turkey as well. Cheese, whole milk, cream, butter and ice cream are examples of dairy foods that may also increase inflammation in the body.
Other Pro-Inflammatory Foods
 Refined grain products and sugars cause a rapid rise in blood sugar levels which, over time, can be detrimental to health and lead to chronic inflammation. The anti-inflammatory diet outlined by The University of Wisconsin Department of Integrative Medicine suggests eliminating white bread, bagels, rolls, cake, cookies, muffins, pancakes, sugary cereals, sweetened drinks and white rice. Opt for whole grain products that are minimally processed instead, such as oatmeal, brown rice and 100% whole wheat breads and cereals that are high in fiber.
Refined grain products and sugars cause a rapid rise in blood sugar levels which, over time, can be detrimental to health and lead to chronic inflammation. The anti-inflammatory diet outlined by The University of Wisconsin Department of Integrative Medicine suggests eliminating white bread, bagels, rolls, cake, cookies, muffins, pancakes, sugary cereals, sweetened drinks and white rice. Opt for whole grain products that are minimally processed instead, such as oatmeal, brown rice and 100% whole wheat breads and cereals that are high in fiber.
Certain Omega 6 polyunsaturated fats may also increase inflammation. Limit intake of corn oil, sunflower oil, safflower oil, and soybean oil; olive and canola oils are healthier choices
Nightshades – Nightshade plants, such as tomatoes, potatoes, eggplant and peppers, is common in the Western diet, but can lead to inflammation in people who respond poorly to the chemicals, called alkaloids, produced when these foods are digested. These alkaloids can lead to systemic irritation and allergic responses that increase inflammation. In the early stages of an anti-inflammatory diet, naturopathic physician James Wilson advocates total avoidance of nightshades, followed by a gradual reintroduction after eight weeks.
More on Omega 6 – Foods High in Omega-6 Fats –Foods high in omega-6 fatty acids increase inflammation in the body by making more arachidonic acid, a chemical directly related to inflammation. Reducing consumption of processed foods like potato chips and snack cakes as well as replacing peanuts, canola oil, soybean oil and margarine in the diet can help reduce inflammation. You can add anti-inflammatory fats found in fish oil to help mitigate the inflammation caused by excessive consumption of omega-6 fats.
Sugary Foods – Sugary foods play a profound role in inflammation, and particularly the activation of inflammation caused by arachidonic acid. Sugary foods lead to a fast spike in blood sugar that causes the pancreas to increase its production of the hormone insulin, leading to the activation of enzymes that facilitate inflammation. Though all carbohydrate-rich foods lead to a rise in blood sugar, foods like beans, whole grains and fresh fruits result in lower levels of blood sugar, making them better options for an anti-inflammatory diet.
Omega 3 Fatty Acids – Omega 3 fatty acids not only have heart-healthy benefits but may help manage other inflammatory diseases such as rheumatoid arthritis. According to the University of Maryland Medical Center, we consume 14 to 25 times more Omega 6 fats than Omega 3s.The University of Wisconsin Department of Integrative Medicine states that a diet high in Omega-6 fatty acids can prevent the body from using Omega-3s. A healthy, anti-inflammatory diet should include plenty of Omega 3 sources including fatty fish such as salmon, herring, mackerel and sardines. Plant sources of Omega 3s include flax seed and oil, walnuts and canola oil.
Other Anti-Inflammatory Foods – Colorful fruits and vegetables contain pigments that contain health-enhancing antioxidants that help to reduce inflammation in the body. Choose dark green leafy vegetables such as spinach, kale and Swiss chard, as well as colorful bell peppers, carrots, sweet potatoes and broccoli. Nuts and seeds may help to lower inflammation a Mediterranean eating type eating plan (Mainly fresh fruits and vegetables) includes the foods necessary to help to prevent and reduce inflammation.
Adding a variety of fresh foods to the diet is beneficial in staying healthy and controlling inflammation and other symptoms of disease. Food that is eaten fresh and in its natural state offers the most nutrients. The nutrients in raw foods are easily assimilated by the body. The storage and preparation of fresh foods is the key in how well they hold their nutritive value. Freezing is a popular way to store fresh foods.
 Weight Loss – Losing weight may be one of the best ways to reduce inflammation and its detrimental health effects. Fat cells produce inflammatory proteins that may play a significant role in disease. Obesity has been linked to a higher risk of heart disease, diabetes, cancers and other diseases, and this may be mediated by increased inflammation. A healthy, eating plan that is designed to lose one or two pounds weekly will help to reduce inflammation and improve health overall.
Weight Loss – Losing weight may be one of the best ways to reduce inflammation and its detrimental health effects. Fat cells produce inflammatory proteins that may play a significant role in disease. Obesity has been linked to a higher risk of heart disease, diabetes, cancers and other diseases, and this may be mediated by increased inflammation. A healthy, eating plan that is designed to lose one or two pounds weekly will help to reduce inflammation and improve health overall.
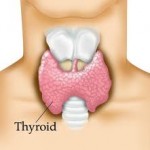 What is Thyroiditis? Thyroiditis is a general term that refers to “inflammation of the thyroid gland”. Thyroiditis includes a group of individual disorders causing thyroidal inflammation but presenting in different ways. For example, Hashimoto’s thyroiditis is the most common cause of hypothyroidism in the United States.
What is Thyroiditis? Thyroiditis is a general term that refers to “inflammation of the thyroid gland”. Thyroiditis includes a group of individual disorders causing thyroidal inflammation but presenting in different ways. For example, Hashimoto’s thyroiditis is the most common cause of hypothyroidism in the United States.
What causes thyroiditis? Thyroiditis is caused by an attack on the thyroid, causing inflammation and damage to the thyroid cells. Antibodies that attack the thyroid cause most types of thyroiditis. As such, thyroiditis is often an autoimmune disease, like juvenile diabetes and rheumatoid arthritis. What are the different types of thyroiditis and how do they affect the body?
There are several types of thyroiditis.
Hashimoto’s thyroiditis – Caused by antibodies that attack the thyroid .Shows symptoms of hypothyroidism. Results in permanent hypothyroidism.
Subacute thyroiditis – (also called de Quervain’s thyroiditis) Possibly caused by a viral infection. Causes pain in the thyroid and symptoms of hyperthyroidism, followed by hypothyroidism. Symptoms improve within a few months. There is a slight chance of permanent hypothyroidism, which can be treated.
Silent thyroiditis – Shows symptoms of hyperthyroidism, followed by hypothyroidism. Symptoms improve within 12 to 18 months. May result in permanent hypothyroidism.
Postpartum thyroiditis – Caused by antibodies that attack the thyroid after delivery of a child. Four to 6 months after delivery, symptoms of hyperthyroidism appear, followed by hypothyroidism. Symptoms improve within 12 to 18 months. May result in permanent hypothyroidism.
Drug-induced thyroiditis – Caused by prescription drugs such as amiodarone, lithium, interferon and cytokines. Shows symptoms of hyperthyroidism or hypothyroidism. Symptoms continue as long as the drug is taken.
Radiation-induced thyroiditis – Follows treatment with radioactive iodine for hyperthyroidism or radiation therapy for certain cancers. Most commonly shows symptoms of hypothyroidism. Hypothyroidism is usually permanent, but can be treated.
Acute thyroiditis – (also called suppurative thyroiditis) Caused by bacteria or other infectious organisms. Symptoms include a painful thyroid, generalized illness and occasionally symptoms of mild hypothyroidism. Symptoms improve after treatment of the infectious cause. Risk Factors for Thyroid Disease
Some of the key risk factors for thyroid disease include…
Female: Women are at greater risk than men. Age – being 50 and above poses the highest risk of thyroid disease, though it can strike at any age. A personal or family history of thyroid and/or autoimmune disease increases risk. Surgical removal of all or part of the thyroid, or radioactive iodine treatment to the thyroid — both which typically result in an underactive thyroid. Being left-handed, ambidextrous or prematurely gray mean greater risk of autoimmune disease, including thyroid problems, Being pregnant or within the first year after childbirth, Current or former smoker, Recent exposure to iodine via contrast dye or surgical antiseptic, Iodine or herbal supplements containing iodine, in pill or liquid form, Living in an iodine-deficient area, Various medical treatments, including Interferon Beta-1b, Interleukin-4, immunosuppressants, antiretrovirals, monoclonal antibody (Campath-1H), bone marrow transplant, Lithium, amiodarone (Cordarone), and other medications, Overconsumption of raw goitrogenic foods, i.e., Brussel sprouts, turnips, cauliflower, soy products and others, Overconsumption of soy foods and soy isoflavones, Recent neck trauma, biopsy, injection or surgery, Radiation exposure, through radiation to neck area, or exposure to nuclear facility or accident, i.e., Chernobyl, High stress life events. Just to name a few.
Blood Tests to Detect Inflammation
 Erythrocyte sedimentation rate, C-reactive protein and plasma viscosity are blood tests that detect inflammation. These are useful tests to help diagnose and monitor the activity of certain diseases.
Erythrocyte sedimentation rate, C-reactive protein and plasma viscosity are blood tests that detect inflammation. These are useful tests to help diagnose and monitor the activity of certain diseases.
If you have inflammation in a part of your body then extra protein is often released from the site of inflammation and circulates in the bloodstream. The erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and plasma viscosity (PV) blood tests are commonly used to detect this increase in protein, and so are markers of inflammation.
Erythrocyte sedimentation rate, C-reactive protein and plasma viscosity blood tests
Erythrocyte sedimentation rate (ESR) – A blood sample is taken and put in a tube that contains a chemical to stop the blood from clotting. The tube is left to stand upright. The red blood cells (erythrocytes) gradually fall to the bottom of the tube (as sediment). The clear liquid plasma is left at the top. The ESR measures the rate at which the red blood cells separate from the plasma and fall to the bottom of a test tube. The rate is measured in millimetres per hour (mm/hr). This is easy to measure as there will be a number of millimetres of clear liquid at the top of the red blood after one hour. If certain proteins cover red cells, these will stick to each other and cause the red cells to fall more quickly. So, a high ESR indicates that you have some inflammation, somewhere in the body. Levels of ESR are generally higher in females and also the level increases with increasing age.
C-reactive protein (CRP) – This is sometimes called an acute phase protein. This means that the level of CRP increases when you have certain diseases which cause inflammation. CRP can be measured in a blood sample.
Plasma viscosity (PV) – The conditions which the ESR test monitors can also be monitored by the PV test. However, it is more difficult to perform and is not as widely used as ESR testing. 1. Stop smoking. Smoking hardens the arteries and could send CRP levels surging. But research shows you can reverse all the damaging effects to your arteries within 10 years of quitting.
6 Ways to Reduce Inflammation—without a dangerous Statin drugs or an  expensive Heart Test
expensive Heart Test
1. Stop smoking. Smoking hardens the arteries and could send CRP levels surging. But research shows you can reverse all the damaging effects to your arteries within 10 years of quitting.
2. Think olive oil, fish, and nuts. Researchers have shown that overweight folks who stick with a Mediterranean-style diet—based on fruits, vegetables, whole grains, nuts, and olive oil—can lower their levels of inflammation. “An anti-inflammatory diet is about reducing saturated fat and trans fats and eating more foods rich in alpha-linolenic acid—like flaxseed, walnuts, and canola oil—and omega-3 fats, which fight inflammation. Scientists have shown that the typical American fast-food diet increases heart attack risk by 30 percent.
3. Get active. No one wants to exercise, but it’s a great way to lower inflammation without any side effects associated with medications. An ideal amount? Not too much (which raises inflammation) and not too little. Aim for five days a week of steady exercise (brisk walking, swimming, biking) for 30 to 45 minutes.
4. Shrink your waist size. Take a tape measure and measure your waist, right around the point of your bellybutton. If you’re a woman with a waist measurement of over 35 inches or a man with a waist of over 40 inches, you probably have high inflammation. Whittling a few inches off the waist by reducing your portions and increasing activity can go a long way toward solving that problem.
5. Get enough sleep. A new study out this week shows that elderly people with high blood pressure who sleep less than 7.5 hours a night have dramatically elevated chances of having a stroke or heart attack or suffering sudden cardiac death. Other research has shown that too little sleep (less than six hours) or too much (more than eight hours) results in more inflammation. The American Academy of Sleep Medicine says most adults need between seven and eight hours of shut-eye a night.
6. Reduce stress. High levels of stress hormones can lead to the release of excess inflammatory chemicals, so try each day to get in 15 to 20 minutes of relaxation—deep breathing, meditation, or a bubble bath that lets you de-compress for the day.
Vitamins that Fight Inflammation
 Eat a healthy diet, is the number one thing to do to fight inflammation. Research is finding that diet can play an important part in reducing inflammation. Certain vitamins in particular may help control inflammatory processes in the body. Which vitamins have the most anti-inflammatory potential? Here’s what the research has to say:
Eat a healthy diet, is the number one thing to do to fight inflammation. Research is finding that diet can play an important part in reducing inflammation. Certain vitamins in particular may help control inflammatory processes in the body. Which vitamins have the most anti-inflammatory potential? Here’s what the research has to say:
Vitamin A – Vitamin A is commonly found in whole milk, liver, and some fortified foods. Beta-carotene is a provitamin found in carrots and many colorful vegetables that can be converted to vitamin A in the body. Vitamin A is an antioxidant. That means it protects against harmful substances in your body called free radicals, which can damage DNA and lead to cancer and other diseases. Vitamin A also has anti-inflammatory effects.
The evidence: A lack of enough vitamin A has been linked to inflammation in the intestines, lungs, and skin. For some people, taking vitamin A supplements could reduce the inflammation that contributes to conditions like inflammatory bowel disease, acne, and lung disease.
Vitamin B6 – This member of the B vitamin family is plentiful in foods like beef, turkey, vegetables, and fish. Because vitamin B6 is water-soluble, your body is constantly ridding itself of it, so you need to restock it daily through diet.
The evidence: Not getting enough vitamin B6 may increase your risk for heart disease. Studies have found that people who lack enough of this vitamin have high levels of C-reactive protein (CRP), a marker of inflammation that has been linked to heart disease.
A lack of vitamin B6 can increase inflammation associated with rheumatoid arthritis, leading to more joint damage. Yet in a vicious cycle, inflammation from rheumatoid arthritis can deplete the body’s vitamin B6 stores. Taking vitamin B6 supplements daily can correct the deficiency, yet researchers say there’s no conclusive evidence it will reduce inflammation too.
Vitamin C – Your body uses this vitamin, found in oranges and other citrus fruits, for a number of different purposes. Vitamin C helps to produce collagen — the building block of skin, cartilage, ligaments, and blood vessels, and it protects against harmful substances that contribute to disease. Vitamin C is an effective antioxidant and studies suggest that it has some anti-inflammatory benefits.
The evidence: Taking vitamin C supplements may significantly lower CRP levels, research finds. Whether having lower levels of this inflammatory marker might translate into a lower risk for heart disease remains to be seen, however.
Vitamin D – The same vitamin that works with calcium to strengthen bones can also protect against inflammation. Vitamin D can be found in fish, liver, beef, egg yolks, and some fortified foods. Vitamin D is also produced in the body when the skin is exposed to sunlight.
The evidence: Vitamin D deficiency has been linked to a number of inflammatory diseases, including rheumatoid arthritis, lupus, inflammatory bowel disease, and type 1 diabetes. Taking vitamin D supplements may help reduce inflammation in people with these conditions, although this hasn’t been proven. Vitamin D deficiency may even increase levels of inflammatory markers in healthy people. Vitamin D supplements may also reduce the inflammation associated with age-related diseases.
One study found that people with the highest vitamin D levels had a 40% lower risk of colon cancer than those who had the lowest level of this vitamin. However, it’s not yet clear whether taking vitamin D supplements can actually lower cancer risk.
Vitamin E – Vitamin E is another antioxidant with anti-inflammatory properties. Common food sources include nuts, seeds, and green leafy vegetables.
The evidence: Vitamin E comes in several different forms. The alpha-tocopherol type may help prevent heart disease by slowing the release of inflammatory substances that damage the heart.
Alpha-tocopherol also might be effective for easing lung inflammation related to allergies. However, because studies were conducted on animals, it’s not yet clear whether the results will translate to humans.
Vitamin K – Vitamin K — found in green vegetables like asparagus, broccoli, kale, and spinach — is best known for its role in helping blood clot, but research is finding that it may have other benefits, too.
The evidence: Getting more vitamin K can reduce levels of inflammatory markers throughout the body.

